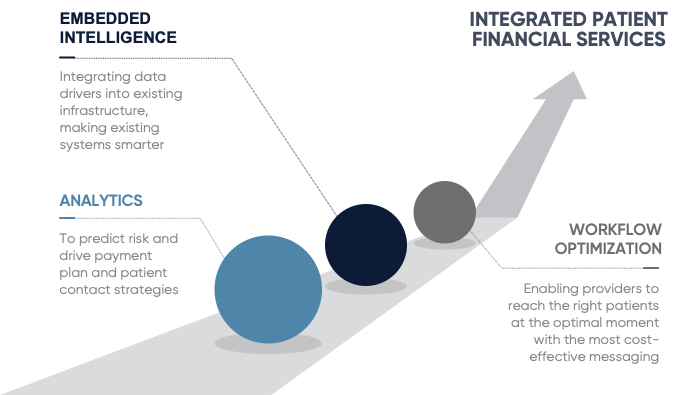
MedData uses Predictive Patient Scoring and Segmenting Technology as an important component of our Patient Responsibility/Early Out Services. With this technology, patient data is scored and segmented with predictive analytics to determine propensity to pay. Highly accurate results inform proactive patient outreach with personalized financial data that simplifies the process and drives faster account resolution. This technology ensures that monthly payment plans are tailored specifically to the patient’s financial situation to encourage best outcomes.
MedData’s Patient Responsibility/Early Out Services take a patient-focused approach to self-pay account resolution, making it simple and easy for patients to pay with many different means to resolve their bills. We also make the overall process as fast and convenient as possible by offering patients a variety of methods to get involved – phone calls, texting, self-service, payment portal – and we’re there if they do need help.
Our philosophy of patient education and compassionate customer service is a key component to our success. We focus on helping patients understand the post-clinical process by providing education on their statement, their balance, and their insurance options.
Our dedicated, U.S.-based patient service center has hundreds of Patient Service Representatives (PSRs) with expansion capacity to scale with our clients’ business and we have bi-lingual staff in our call center and translation support for multiple languages.
We have a First Call Resolution rate that consistently exceeds 90%. The first time we speak with a patient, we do whatever we can to solve their issue right then. That could mean taking payment in full, setting up a payment arrangement, or calling an insurance company together to help walk the patient through what’s taken place.
Our operations and patient pay management system empowers PSRs to have the right information at the right time to customize each call per client and patient. MedData’s PSRs are trained to handle all types of accounts to ensure increased call volume scenarios are handled well within our aggressive quality control requirements.
Patients can be overwhelmed by multiple hard-to-understand bills from different sources. We consolidate their bills and provide an intuitive statement to eliminate confusion and make it easy to understand what they owe. Our statements are designed to incorporate client branding and color coded according to urgency – green for timely statements, orange for late statements, and red for statements close to being sent to collections.
Our propensity to pay tool uses hundreds of demographic data points to identify patients where additional communication and education can help resolve accounts sooner, as well as what format to use – hard copy statement, phone call, text, etc. The scoring system also can be built to fit contractual recommendations from the client. This technology ensures that monthly payment plans are tailored specifically to patient’s financial situation to encourage best outcomes, and it does not impact the patient’s credit report.
With our patient texting technology, you can send first statements directly to patients’ smartphones. It’s much faster than mailing a paper statement and requires less effort for patients to respond, which helps drives patient engagement and improve collections. Our online payment portal is designed to streamline patient balance reimbursements and give patients greater insight into the medical billing process. It consolidates all payments and balances into an easy-to-read dashboard. Our technology also lets providers view all accounts associated with a guarantor, receive documentation, and accept payments in real time.
We connect and engage with patients throughout the entire patient financial life cycle, treating them with dignity and respect, and providing opportunity for dialogue and to learn more all along the way.