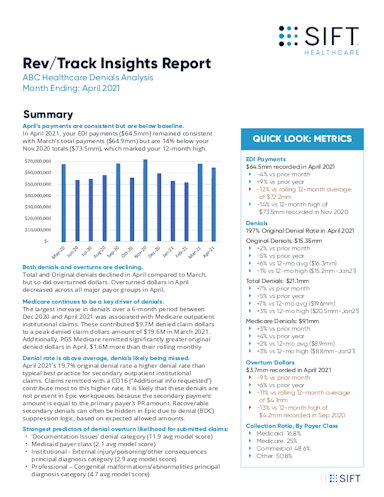
Unprecedented access to your payments data. Sift’s Rev/Track reporting dashboards and Insights Reports deliver custom, enhanced operational intelligence that enables better benchmarking and data-driven decision-making. Sift's Rev/Track tools provide a comprehensive analysis of historical and current billed procedures, forecasting how payments will perform as a result of current payer and payment trends – and what can be done to improve outcomes.
Access and learn from your data at any time with Sift’s Rev/Track command center. Sift’s dynamic Rev/Track dashboards provide detailed, granular reporting for all levels within a provider organization, from the C-Suite to functional team leaders.
- Full lifecycle view, tracking the impact of every claim
- Early warning system – trend tracking and alerts
- Payer Scorecards
- Portfolio views of payments, covering both Payers and Patients
Delivery of a complete picture of your payment behavior. Sift's detailed Rev/Track Insights Reports serve as actionable analyst reports that highlight trends, problems and opportunities that directly impact revenue.
Sift integrates clinical and coding data to enhance root cause analytics. Sift predicts the weighted contributions of upstream clinical workflow data inputs by tying together concurrent and back-end denial and overturn patterns. This enables deep drill-downs of the clinical and account data that contribute to predicted denials.