A health system is looking for ways to drive more patients to their cardiology service line. Historically, cardiology has been one of their more profitable service lines. With a provider network featuring multiple facilities and other service lines, the system has struggled to track the downstream progress of a patient after their primary care referral.
Leveraging Care Continuity's PCP-to-Specialist Referral Management solution, a data feed of referrals is sent to Care Continuity where the software's AI uses dozens of data points -- including diagnoses, discharge notes, patient information, social determinants of health, and more -- as well as a set of customizable prioritization rules to create a navigation queue for a team of expert navigators to personally contact and navigate.
This allows for a multi-dimensional approach to patient navigation that can predict which patients are most in need of, as well as open to, navigational assistance.
The trained team of navigators contact the patients based on their priority ranking and can coordinate the specialist appointment between both patient and office. On average, a patient navigator can schedule a higher percentage of appointments at a faster rate when compared to other self-navigation methods. In addition, appointments scheduled via a patient navigator are statistically less likely to result in a no-show.
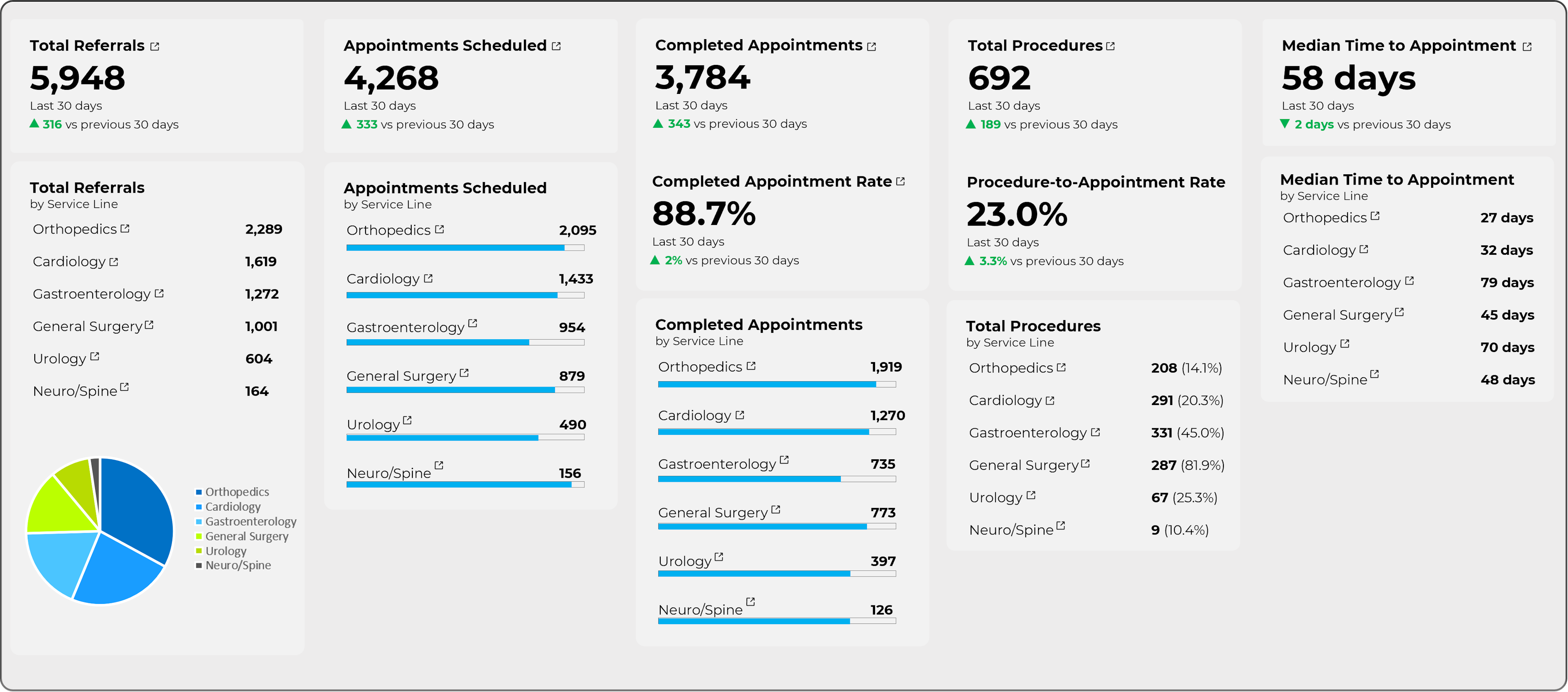
After the program is implemented, health system stakeholders receive a data dashboard that shows the downstream impact of the navigation, including the total number of appointments scheduled, the number of completed appointments, the number of appointments that required procedures, and median time to appointment.
With this data broken down by both service line and facility, a health system can focus on a profitable service line such as Cardiology, looking for areas to improve their network and make a positive financial impact.